Understand The Science Of Teeth Whitening
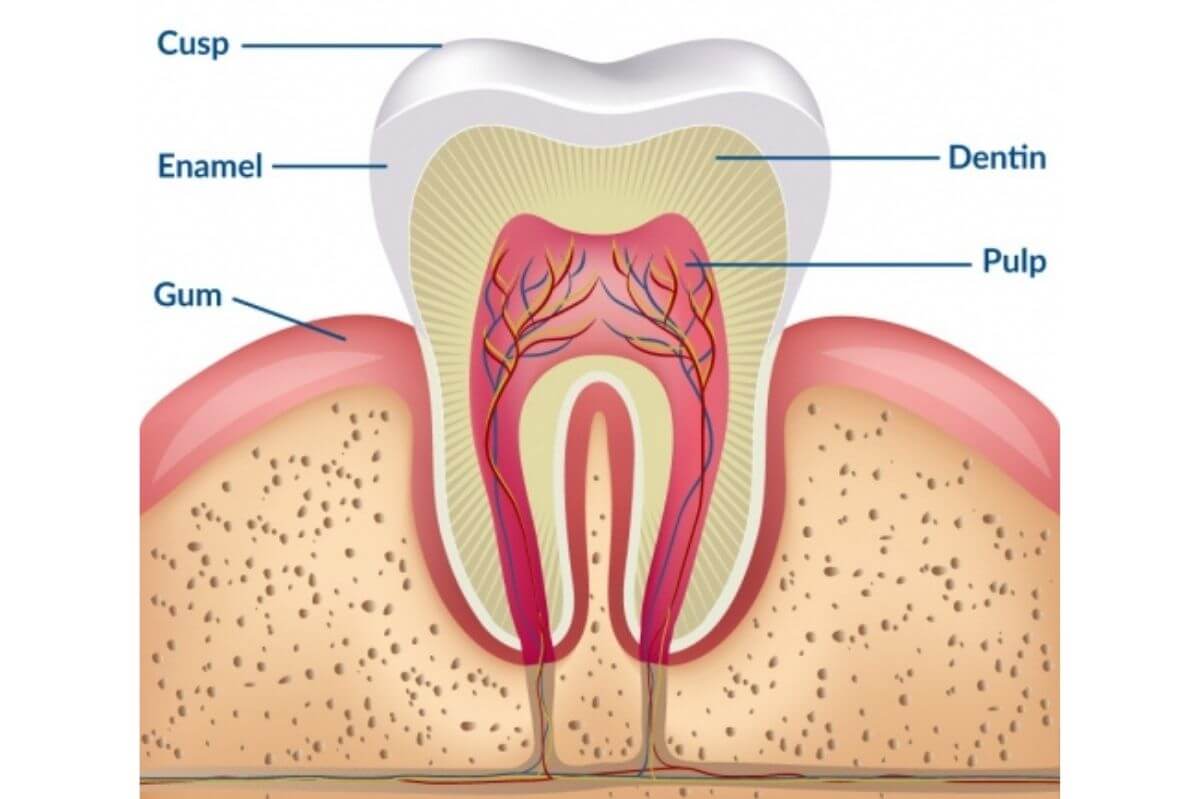
Teeth whitening—often referred to as dental bleaching—is the process of lightening the color of your teeth by removing or altering the stains that reside on and within the enamel and dentin layers of the tooth . In both professional settings and at‑home kits, whitening agents such as hydrogen peroxide and carbamide peroxide break down chromogens (pigmented molecules) via oxidation, transforming them into smaller, less‑colored compounds that reflect less light and thus appear whiter . This article dives into the mechanisms, methods, safety considerations, and aftercare of modern teeth whitening.
WHAT IS TEETH WHITENING?
Teeth whitening is the application of bleaching agents to alter the intrinsic or extrinsic coloration of natural tooth structure .
Extrinsic stains form on the enamel surface through exposure to pigmented foods, drinks, tobacco, and poor oral hygiene. These are often removable by mechanical cleaning or low‑concentration whitening toothpastes .
Intrinsic stains develop within the enamel or dentin due to factors like fluorosis, tetracycline exposure, aging, or trauma; these require chemical bleaching to penetrate the tooth and oxidize the embedded chromogens .
THE CHEMICAL MECHANISM OF BLEACHING
Oxidative Breakdown
Hydrogen peroxide (H₂O₂) or its precursor carbamide peroxide diffuses through enamel’s interprismatic spaces and dentinal tubules .
In contact with water, carbamide peroxide releases one‑third of its content as H₂O₂, which then yields reactive oxygen species (free radicals) .
These free radicals attack unsaturated bonds in organic chromophores, cleaving them into smaller, less pigmented molecules .
Influencing Factors
pH & Temperature: Optimal pH and mild heat can accelerate peroxide decomposition and stain removal, though excessive heat risks pulp irritation .
Light Activation: Some in‑office systems use halogen, LED, or plasma arc lights to speed bleaching, though benefits over non‑light protocols are marginal and may increase sensitivity .
WHITENING AGENTS & CONCENTRATIONS
At‑Home Kits: Typically contain 10–22% carbamide peroxide (≈3–7% hydrogen peroxide) for overnight or daytime wear; marketed for convenience and reduced sensitivity .
In‑Office Treatments: Use 25–40% hydrogen peroxide under professional supervision, often combined with light, to achieve 2–8 shades of whitening in a single session .
Regulatory Limits: Over‑the‑counter H₂O₂ products in many regions are capped at ~6% to ensure safety, while stronger formulations require dental professional administration .
PROFESSIONAL VS. AT‑HOME METHODS
| Feature | In‑Office | At‑Home |
|---|---|---|
| Peroxide Concentration | 25–40% H₂O₂ | 3–7% H₂O₂ (via carbamide peroxide) |
| Activation | Optional light/heat | Tray‑based or strip‑based |
| Treatment Time | 30–60 minutes (single visit) | 30–90 minutes per day over 1–2 weeks |
| Results | 3–8 shades lighter in one session | 1–3 shades lighter per week |
| Sensitivity Risk | Higher (transient; managed in office) | Lower (spread over multiple applications) |
Professional treatments offer rapid, dramatic results, while at‑home systems balance efficacy with convenience and gentler peroxide levels .
SAFETY & COMMON SIDE EFFECTS
Tooth Sensitivity: Transient hypersensitivity arises as dentinal tubules open; affects up to 78% of in‑office patients and ~50% of at‑home users, usually resolving within days .
Gingival Irritation: Mild bleaching solution contact can blanch and sting gums; custom‑fit trays and careful application minimize leakage .
Restoration Effects: Peroxides can weaken composite resins and increase amalgam ion release temporarily; patients with multiple crowns or veneers should be counseled on potential shade mismatch .
Overuse Risks: Frequent or prolonged bleaching may erode enamel, increase porosity, and lead to a translucent appearance if misused .
Try Lidercare Now!
We Help You Launch New Products, And Continue To Grow. Try Us With 20% Off Your First Order!
POST‑TREATMENT CARE & REMINERALIZATION
After bleaching, enamel micro‑tubules remain open; applying a remineralizing gel containing calcium phosphate and fluoride helps reseal tubules, reduce sensitivity, and “lock in” whitening results . Some protocols recommend:
Using a desensitizing gel (e.g., potassium nitrate) for 5–10 minutes post‑treatment .
Following a “White Diet” (avoiding staining foods/drinks) for 24–48 hours to optimize uptake .
MAINTAINING YOUR WHITER SMILE
Oral Hygiene: Brush twice daily with a whitening toothpaste to manage extrinsic stains .
Diet & Lifestyle: Limit coffee, tea, red wine, and tobacco; use a straw for dark beverages; rinse or brush promptly after consumption .
Touch‑Ups: Periodic at‑home bleaching or professional in‑office boosters every 6–12 months help sustain results .
FREQUENTLY ASKED QUESTIONS
Is teeth whitening safe for enamel?
Yes—when used as directed, peroxide concentrations under professional supervision do not cause lasting enamel damage; transient sensitivity is the most common effect .How long do whitening results last?
Typically 6–12 months, depending on diet, oral hygiene, and smoking habits; maintenance touch‑ups extend longevity.Does whitening work on all types of stains?
Works best on yellow or brown stains. Grayish or tetracycline‑induced stains may require extended treatment or restorative options .How often can I safely whiten my teeth?
Professional‑strength at home: every 6–12 months. In‑office treatments: up to twice yearly, based on sensitivity and enamel health .Can I whiten over dental restorations?
No—bleaching agents do not change the shade of fillings, crowns, or veneers; plan for restoration replacement after bleaching for shade matching .What should I do if I experience severe gum irritation?
Rinse thoroughly, discontinue treatment, and consult your dentist; custom trays and lower‑concentration gels help prevent recurrence
Table of Contents
Awesome! Share to:
Latest Blog Posts
Check out the latest industry trends and take inspiration from our updated blogs, giving you a fresh insight to help boost your business.